Table of Contents
Fertility Test
Don’t take your fertility health for granted. This at-home blood and saliva Fertility Test by Thorne provides insights by measuring a woman’s reproductive hormones, thyroid function, and stress responses. Fertility Test results include a personalized health.
You should take this Fertility Test if you
- Plan to get pregnant someday
- Are trying to conceive
- Have irregular or no periods
- Experience persistent stress
- Want to understand your hormones
- Have family thyroid issues
What you’ll discover

Measures
Your personal biomarker values are displayed on an easy-to-read dashboard with descriptions of what each biomarker value means for you.

Analysis
Using your biomarkers, we provide detailed insights to help identify potential health risks or specific areas of improvement. Insights are generated using Thorne’s Health Intelligence platform.

Improvement Plan
Based on your unique Fertility Test results, a comprehensive improvement plan with diet, activity, and supplement recommendations is generated.
What we measure
How it works

1 • Order and activate
After your purchase is complete, everything you need for your at-home Fertility Test is delivered to your door. Use the activation code located on the back of the Fertility Test kit to activate your test on thorne.com and complete your health profile.

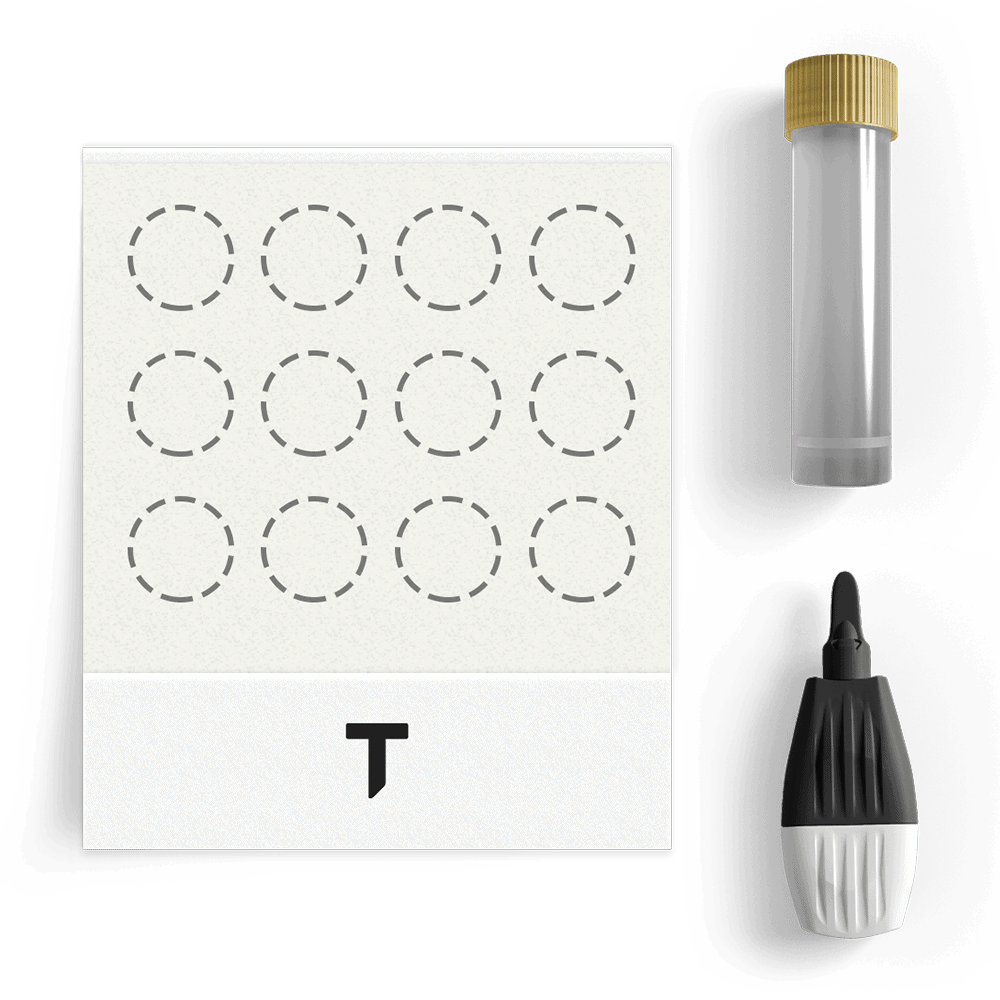
2 • Collect samples and send
Referencing the directions booklet included in your Fertility Test kit, complete your sample collection from the comfort of your home. Use the prepaid shipper to mail your samples directly to the laboratory.

3 • Receive results and recommendations
Your results will be reviewed by an independent, board-certified physician. Once you’ve sent your samples to the lab, after 8-10 business days you will receive your Fertility Test results with meaningful insights and personalized recommendations by one of our health coach professionals to promote your health and wellness.
Potential Fertility Test Indicators
Symptoms attributable to an imbalance of fertility-related hormones can include the following:
- Skin changes, including acne
- Dark hair growth on the lips, chest, and chin
- Loss or thinning of hair
- Unexplained weight gain
- Breast tenderness
- Hot flashes
- Night sweats
- Changes in sex drive and desire, including reduced libido
- Mood changes
- Irregular or no periods
- Sleep difficulty
- Fatigue
- Infertility
Fertility Test 101
Aspects of fertility
Human fertility is measured by being able to successfully conceive. Infertility is the inability of a woman to conceive after one year of trying to do so. Although infertility is relatively common, those struggling with it are nevertheless confronted with medical, psychological, and financial uncertainty, which can be highly frustrating.
But there are actions that can be taken to improve fertility. The Thorne Fertility Test provides an assessment that reflects the convergence of biological, psychological, and social elements. This Fertility Test assessment, when combined with proven methods to improve your diet, nutrition, stress, sleep, activity level, and other factors, can empower you and promote healthy fertility.
Human fertility is a complex process that is affected by a wide variety of factors. Alterations in the biological status of these factors can contribute to infertility. Factors that have been shown to affect fertility include:
- Age
- Diseases or disorders
- Genetics
- Hormones
- Sleep patterns
- Stress
- Nutrition
- Environmental toxins
- Exercise and activity level
- Weight and level of body fat
How the biomarkers we measure impact your health
Fortunately, there are evidence-based steps that can be taken to improve your chances to conceive. The Thorne Fertility Test analyzes three groups of hormones that have been shown to impact fertility ‐ reproductive hormones, thyroid hormones, and adrenal hormones. These hormones work synergistically in the body to promote or impede fertility.
And certain biological markers, when they are out of normal range, can contribute to infertility more than others.
The test panels in the Thorne Fertility Test are not intended to be used as diagnostic measures relative to determining your fertility. Instead, this test is intended to be a screening tool, that is within your control, that will reveal patterns in your hormones that might be influencing your fertility.
With a knowledge of these patterns, you can then take basic supportive steps and more precisely communicate with your health-care practitioner.
Reproductive Hormones
Estradiol
Estradiol, the most powerful and active form of estrogen, plays a critical role in fertility. Estrogen stimulates maturation of an egg and, after ovulation, causes the uterine lining to thicken in preparation for implantation of a fertilized egg.
Progesterone
Progesterone is released by the ovaries in response to ovulation. After ovulation, progesterone levels rise to prepare the uterine lining to accept and nourish a possible fertilized egg. A low progesterone level can make it difficult to sustain a pregnancy.
Testosterone
Testosterone, typically thought of as the “male hormone,” is also needed in a small quantity for good reproductive health in women. Too little or too much testosterone can disrupt fertility. In fact, a high testosterone level is most associated with infertility related to Polycystic Ovarian Syndrome.
Follicle-stimulating hormone (FSH)
FSH is secreted by the pituitary gland in the brain and stimulates the growth of ovarian follicles, the maturation of an egg within the follicle, and the secretion of estrogen and progesterone. It is instrumental in helping maintain the menstrual cycle.
Luteinizing hormone (LH)
LH is the trigger hormone for ovulation. When an ovarian follicle secretes enough estrogen, a surge of LH stimulates the release of an egg and development of the corpus luteum (what the ovarian follicle turns into after ovulation).
Thyroid Hormones
Thyroid-stimulating hormone (TSH)
TSH is produced in the pituitary gland in the brain and moves to the thyroid gland just above the collarbone. In the thyroid gland, TSH activates the production of the thyroid hormones, T4, and to a lesser extent, T3. Abnormal levels of TSH are often the first sign of thyroid dysfunction and can contribute to fertility problems.
Triiodothyronine (T3)
T3 is one of two thyroid hormones. Although the thyroid gland produces some T3, the majority of T3 is made from the conversion of T4 to T3 outside the thyroid gland (referred to as peripheral conversion). T3 is more potent than T4 ‐ meaning it has a stronger action on tissues that have thyroid hormone receptors. T3 influences reproduction ‐ too much or too little of it can interfere with the menstrual cycle and prevent normal ovulation.
Tetraiodothyronine; Thyroxine (T4)
T4 is the primary thyroid hormone produced in the thyroid gland. Of the two thyroid hormones, T4 is made in the greatest quantity in the thyroid gland. Although T4 has the same actions as T3, it is not as potent as T3. T4 can be converted to T3.
Thyroid peroxidase antibodies (TPOAbs)
TPOAbs are proteins that can attack thyroid peroxidase (TPO), an important enzyme for thyroid hormone production. The presence of TPOAbs can (but not definitively) indicate an autoimmune-related thyroid dysfunction. TPOAbs are an independent risk factor for having an increased difficulty in becoming pregnant and for loss of pregnancy.
Adrenal Hormones
Cortisol
Cortisol, often referred to as the “stress hormone,” normally has a daily rhythm that peaks 30-60 minutes after waking up and then gradually falls throughout the day. When you have a healthy cortisol level, it helps wake you up in the morning, regulates your energy and hunger, and modulates your normal response to physical and emotional stress throughout the day.
The level of cortisol naturally increases during pregnancy and is important for maintaining a normal pregnancy because it helps regulate immune functions that are important for the fertilized egg to implant in the uterine wall. On the other hand, a persistently elevated cortisol level can alter levels of reproductive hormones and inhibit normal ovulation.
Dehydroepiandrosterone (DHEA)
DHEA is a hormone made in the adrenal glands ‐ and in small amounts in the ovaries and testes. Because DHEA is a precursor to both testosterone and estrogen, either too high or too low a level can significantly impact fertility. In a woman, her DHEA level tends to peak during late adolescence and begins declining naturally around age 30.
A low level of DHEA can make it difficult to become pregnant because DHEA promotes healthy eggs and embryos. In fact, studies show that a healthy level of DHEA improves fertility in women with diminished ovarian reserves. On the other hand, because DHEA is easily metabolized to testosterone, a high level can be associated with PCOS-related infertility.




Reviews
There are no reviews yet.